0
A Woman With Unintended Weight Loss and a Goiter
Posted by Unknown
on
Saturday, April 02, 2011
in
Science Medicine
 A 61-year-old woman presents to the emergency department (ED) after being referred from her primary care provider's (PCP) office for evaluation of tachycardia. She had been seen by her PCP for routine placement of a purified protein derivative (PPD) tuberculin skin test and was incidentally noted to have a pulse of 160 bpm. The patient currently denies any specific complaints other than occasional palpitations. On review of her systems, however, she notes having night sweats; a 110-lb (50-kg) weight loss over the preceding 12 months; and 2-3 months of anxiety, diarrhea, and occasional diplopia. She denies having any fever, chills, chest pain, dyspnea, or swelling in her extremities. She has a past medical history of an unspecified thyroid problem. She does not take any daily medications and has no medication allergies. She has a 50-pack-year smoking history, with occasional alcohol consumption. She had been homeless for a period of time but is currently living in an apartment.
A 61-year-old woman presents to the emergency department (ED) after being referred from her primary care provider's (PCP) office for evaluation of tachycardia. She had been seen by her PCP for routine placement of a purified protein derivative (PPD) tuberculin skin test and was incidentally noted to have a pulse of 160 bpm. The patient currently denies any specific complaints other than occasional palpitations. On review of her systems, however, she notes having night sweats; a 110-lb (50-kg) weight loss over the preceding 12 months; and 2-3 months of anxiety, diarrhea, and occasional diplopia. She denies having any fever, chills, chest pain, dyspnea, or swelling in her extremities. She has a past medical history of an unspecified thyroid problem. She does not take any daily medications and has no medication allergies. She has a 50-pack-year smoking history, with occasional alcohol consumption. She had been homeless for a period of time but is currently living in an apartment.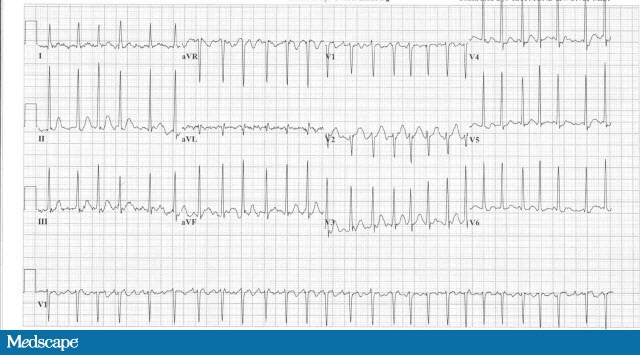
Physical Examination:
- Patient is awake and fully oriented. She is diaphoretic but in no apparent distress.
- Her temperature is 36.1°C; her pulse is 160 bpm; her respiratory rate is 24 breaths/min, with an oxygen saturation of 98%; and her blood pressure is 190/117 mm Hg.
- She has bilateral exophthalmos with exotropia of the right eye (Figure 1). Her visual acuity and extraocular movements are intact.
- The neck examination reveals a diffuse, nontender goiter, without nodules or thyroid bruits.
- The heart is tachycardic, intermittently irregular, and without murmurs.
- The lungs are clear to auscultation bilaterally.
- The abdomen is nondistended, soft, and nontender, with no palpable masses.
- There is no edema of the extremities.
- The neurologic examination reveals normal mentation, intact cranial nerves, intact motor strength and sensation, and normal reflexes. No tremor is noted.
Laboratory Studies: Complete blood count, electrolytes, renal function, and cardiac marker findings are all within normal limits.
Imaging: A plain chest radiograph is interpreted as normal (not pictured). An electrocardiogram (ECG) is obtained (see Figure 2).
Discussion:
Along with bilateral exophthalmos and left exotropia seen on the physical examination, this patient's ECG showed atrial fibrillation with a rapid ventricular response, which is a possible cardiac manifestation of thyrotoxicosis. No ischemic changes were noted despite her rapid heart rate. Her laboratory studies confirmed the suspected diagnosis, with findings of a markedly depressed thyroid-stimulating hormone (TSH) of 0.006 mIU/L (normal range, 0.5-5.0 mIU/L) and elevated triiodothyronine (T3) and thyroxine (T4) concentrations of 9.73 nmol/L and 305.02 nmol/L, respectively.
This patient's clinical presentation bordered between thyrotoxicosis and thyroid storm, and she was hemodynamically stable. She was immediately treated with propranolol and PTU and was admitted to a monitored bed in the medical service. Because her clinical condition improved and she remained stable, the admitting team chose to forgo further therapy with iodine and steroids. Her atrial fibrillation resolved within 12 hours, but an echocardiogram revealed cardiomyopathy with a left ventricular ejection fraction of 45% that was attributed to her long-standing hyperthyroidism. A diagnosis of Graves disease was made. She was continued on methimazole and metoprolol, and anticoagulation was initiated. Five months later, the patient was still taking methimazole. Her thyroid function had normalized, her cardiomyopathy had reversed, and her anticoagulation was discontinued, because atrial fibrillation did not recur. Incidentally, she was ruled out for tuberculosis during her admission with 3 induced sputum samples.
From Medscape